Transcranial Magnetic Stimulation (TMS) therapy is a ground-breaking, non-invasive, low-risk neuromodulatory technique that uses magnetic pulses to stimulate specific areas of the brain and/or body to facilitate recovery.
Transcranial Magnetic Stimulation generates a magnetic field at regular intervals that safely penetrates the head or body leading to a direct effect on the nervous system, also known as neuromodulation. By utilizing excitatory or inhibitory impulses to produce the desired result, it has shown promise for many neurological and psychiatric conditions.
Extensive medical research studies have been performed with TMS leading to Health Canada approval for clinical use in 2002 and FDA approval in 2008.
TMS does not require any anesthesia or hospitalization and there is no restriction on activity.
DR. KALEEL DISCUSSES TMS

PATIENT ELIGIBILITY / CONTRAINDICATIONS
This will be reviewed with you first by your referring provider and subsequently by our nursing staff to ensure your safety.
Patients with intracranial foreign metal bodies or implanted metal devices in the head within 12 inches, or 30 centimeters, of the TMS coil should not receive TMS.
Other considerations would include cardiac pacemakers/defibrillators, aneurysm clips/coils, facial tattoos, history of seizures, serious head injury within the last year, or known history of increased intracranial pressure.
Patients should continue any outpatient medications during treatment and remain stable on their regimen for at least four weeks prior to obtaining treatment with TMS.


THE TREATMENT PROCESS
After receiving your referral, an assessment will be scheduled with our physician who will review your past medical history/treatments. As TMS therapy may be customized for each individual patient, the assessment will determine the optimal location and protocol for your treatment plan. Of note, the patient otherwise remains under the care of the referring physician- TMS assessment and treatment do not constitute a general neurology evaluation and any medication adjustments or other options for treatment, beyond what is offered at HeadworX Clinic, remain under the guidance of the referring physician.
Thereafter, you will be asked to sit in a comfortable, adjustable chair in our treatment room while the technologist performs several measurements of the head or body to localize the treatment area and you will be provided ear plugs. Your motor threshold may be determined during this time- you may notice a slight, painless contraction of your thumb as the impulse is generated- this is the interplay of TMS and your brain at work!
The TMS coil will then be placed on the treatment area by our specialized technologist(s) who will then administer the treatments under the supervision of the neurologist. This generally takes anywhere from 10-30 minutes. The HeadworX Clinic is excited to share that our state-of-the-art machine is fully upgraded with the revolutionary theta burst protocol for eligible patients.
After treatment is completed for the day, you may otherwise carry on with your daily activities as usual.
While rare, any persistent side effects should be immediately brought to the attention of the technologist/nurse. You should also review your ongoing progress with your doctor.
TREATMENT FREQUENCY

Initiation Phase
Treatments are scheduled Monday to Friday, excluding statutory holidays.
20-30 treatments are performed over a 4 to 6 week period- this will be determined by the neurologist. Treatments do not have an immediate effect. Most patients begin to feel a response after the first 1-2 weeks while others are late responders and experience improvement later in the treatment course. Unfortunately, a positive response is not guaranteed.

Maintenance Phase
Maintenance therapy may be helpful in avoiding a relapse. You may return for further treatments after the initial phase- feel free to discuss this with the technologist/nurse, neurologist, or your referring physician.
FAQs
FOR PATIENTS
We accept referrals, review eligibility, and consider TMS treatment for patients suffering from:
– Memory Loss
– Chronic pain including fibromyalgia, migraine, myofascial pain syndrome, low back pain, radiculopathy, complex regional pain syndrome, phantom pain, pelvic pain, peripheral neuropathy, concussion, post-surgical pain, among others.
– Stroke deficits such as weakness or aphasia
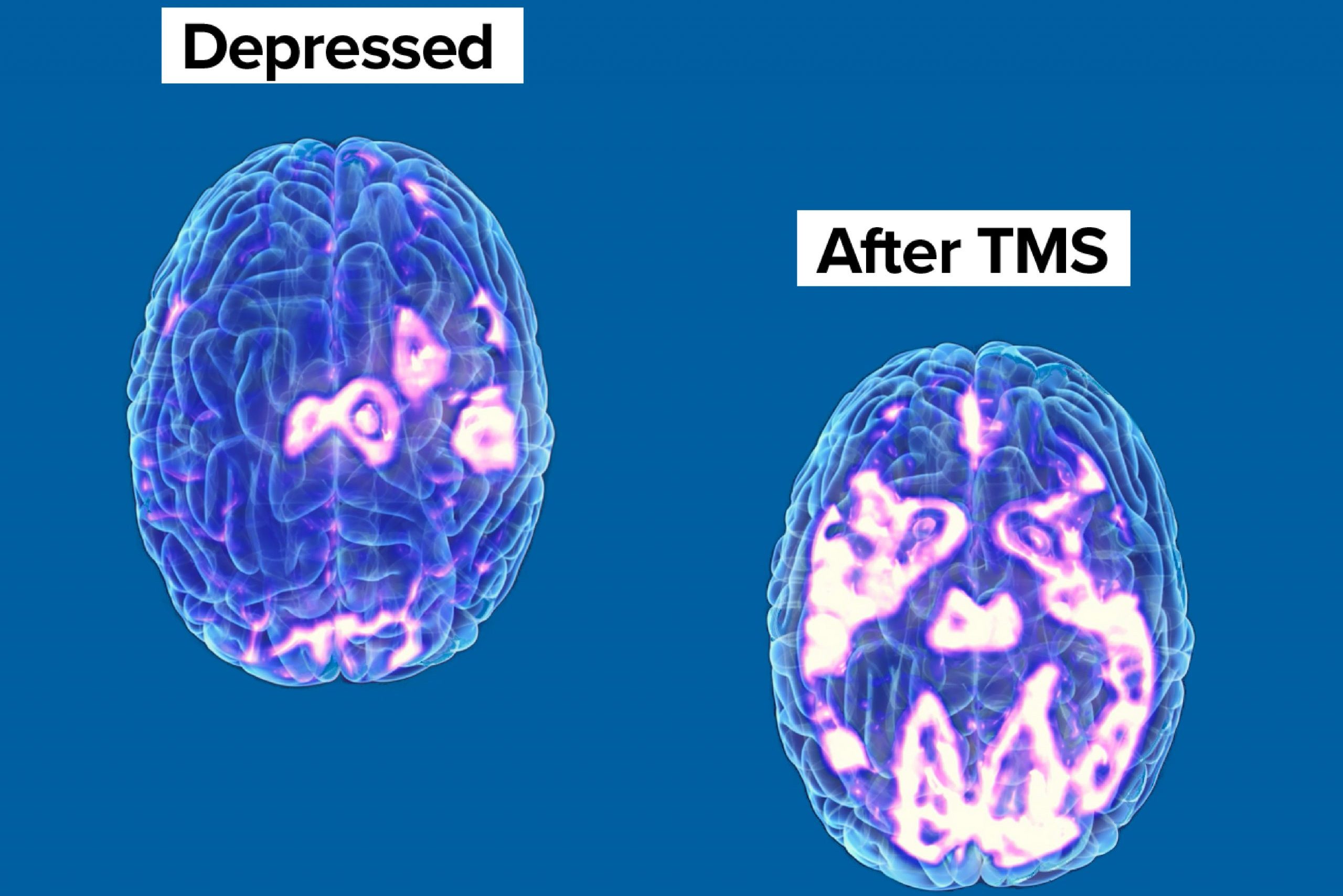
– Depression
– Obsessive Compulsive Disorder
– Weakness or sensory loss following injury or nerve disorders
– Schizophrenia
– Tremor or Parkinson’s disease
– Tinnitus
– Smoking
– Autism Spectrum Disorder
– Post Traumatic Stress Disorder
A referral may be placed by one of your providers i.e. family doctor, psychiatrist, or other healthcare professionals such as a psychologist.
Please call our clinic to discuss. TMS is not currently covered under provincial health plans (OHIP) in Ontario.
You will be provided a receipt of your TMS treatments for your employee benefits plan or income tax return.
Please contact your insurance provider to determine if TMS is covered. It is your responsibility to submit any expenses to your insurance company.
There will be no refund for completed treatment sessions
FAQs
FOR PHYSICIANS AND HEALTH CARE PROFESSIONALS
Our team will review the patient’s history and medications and will explain the process with the patient, including the intended protocol and desired site of stimulation. A consultation note will be provided to your office as well.
Patients will be asked to complete a questionnaire prior to and following the treatment to determine if there has been any change in their status.
While these will be reviewed during the initial consultation, the patient should present to the clinic having been stable on their current medications for at least four weeks. No medication alterations will be made within our TMS clinic and the patient remains under the care of their referring physician. TMS consultation and treatment does not substitute for a general neurology consultation and a separate referral is recommended for any separate neurologic indications.
Please complete our referral form which is available on our website and fax to (226) 647-1010. Referrals are also accepted by the Ocean eReferral Network.
Patients may be referred back to The HeadworX Clinic for another course of treatment.
